Overview
The dermatologic manifestations of either toxic epidermal necrolysis or Stevens-Johnson syndrome may constitute a true emergency. Toxic epidermal necrolysis, an acute disorder, is characterized by widespread erythematous macules and targetoid lesions; full-thickness epidermal necrosis, at least focally; and involvement of more than 30% of the cutaneous surface. Commonly, the mucous membranes are also involved. Nearly all cases of toxic epidermal necrolysis are induced by medications, and the mortality rate can approach 40%.[1]
Manifestations of Stevens-Johnson syndrome include purpuric macules and targetoid lesions; full-thickness epidermal necrosis, although with lesser detachment of the cutaneous surface; and mucous membrane involvement. As with toxic epidermal necrolysis, medications are important inciting agents, although Mycoplasma infections may induce some cases. The mortality rate is much lower than in toxic epidermal necrolysis, approaching 5% of cases.
The prognosis in these diseases is largely a function of the degree of skin sloughing. As the percentage of skin sloughing increases, the mortality rate dramatically worsens. For unknown reasons, however, the disease process in some patients simply stops progressing, and rapid epithelialization ensues. For patients experiencing sloughing over a large area of their skin surface, the mortality rate is much higher. (See the images below.)
 Note early cutaneous slough with areas of violaceous erythema.
Note early cutaneous slough with areas of violaceous erythema.  Extensive sloughing on the face.
Extensive sloughing on the face.  Extensive sloughing on the back.
Extensive sloughing on the back. Together, Stevens-Johnson syndrome and toxic epidermal necrolysis may represent a spectrum of a single disease process. Stevens-Johnson syndrome may also have features of the dermatologic condition erythema multiforme (which has led to confusion in nosology).
Treatment
Only early transfer to and care in a burn unit has been demonstrated to decrease mortality. Coupled with early withdrawal of offending agents, this intervention is the best treatment that can be offered at this time.[2, 3]
Patient History and Physical Examination
Constitutional symptoms, such as fever, cough, or sore throat, may appear 1-3 days prior to any cutaneous lesions. Patients may complain of a burning sensation in their eyes, photophobia, and a burning rash that begins symmetrically on the face and the upper part of the torso. Delineation of a drug exposure timeline is essential, especially in the 1-3 weeks preceding the cutaneous eruption.
Primary lesions
The initial skin lesions of Stevens-Johnson syndrome/toxic epidermal necrolysis are poorly defined, erythematous macules with darker, purpuric centers. The lesions differ from classic target lesions of erythema multiforme by having only 2 zones of color: a central, dusky purpura or a central bulla, with a surrounding macular erythema. A classic target lesion has 3 zones of color: a central, dusky purpura or a central bulla; a surrounding pale, edematous zone; and a surrounding macular erythema. (See the image below.)
 Note the presence of both 2-zoned atypical targetoid lesions and bullae.
Note the presence of both 2-zoned atypical targetoid lesions and bullae. Lesions, with the exception of central bullae, are typically flat. (Lesions of erythema multiforme are more likely to be palpable.) Less frequently, the initial eruption may be scarlatiniform. Flaccid blisters are typically present with full-thickness epidermal necrosis. (See the images below.)
 Extensive blistering and sloughing on the back.
Extensive blistering and sloughing on the back. 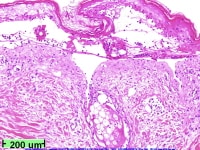 Low-power view showing full-thickness epidermal necrosis.
Low-power view showing full-thickness epidermal necrosis. Nondenuded areas have a wrinkled paper appearance. A Nikolsky sign is easily demonstrated by applying lateral pressure to a bulla. With regard to the arrangement of lesions, individual macules are found surrounding large areas of confluence. (See the image below.)
 Note extensive sloughing.
Note extensive sloughing. Distribution
Lesions begin symmetrically on the face and the upper part of the torso and extend rapidly, with maximal extension in 2-3 days. In some cases, maximal extension can occur rapidly over hours. Lesions may predominate in sun-exposed areas.
Full detachment is more likely to occur in areas subjected to pressure, such as the shoulders, the sacrum, or the buttocks. Painful, edematous erythema may appear on the palms and the soles. The hairy scalp typically remains intact, but the entire epidermis, including the nail beds, may be affected. (See the image below.)
 Sheetlike desquamation on the foot in a patient with toxic epidermal necrolysis. Courtesy of Robert Schwartz, MD.
Sheetlike desquamation on the foot in a patient with toxic epidermal necrolysis. Courtesy of Robert Schwartz, MD. A classification proposes that epidermal detachment in Stevens-Johnson syndrome is limited to less than 10% of the body surface area (BSA). Overlapping Stevens-Johnson syndrome/toxic epidermal necrolysis has more extensive confluence of erythematous and purpuric macules, leading to epidermal detachment of 10-30% of the BSA. Classic toxic epidermal necrolysis has epidermal detachment of more than 30%.
An uncommon form of toxic epidermal necrolysis (toxic epidermal necrolysis without spots) lacks targetoid lesions, and blisters form on confluent erythema. Greater than 10% epidermal detachment is required for diagnosis of these cases.
In contrast, bullous erythema multiforme, which was previously grouped with Stevens-Johnson syndrome, may have epidermal detachment of less than 10% of the BSA, but typical target lesions or raised atypical targets are localized primarily in an acral distribution.
Areas of denuded epidermis in Stevens-Johnson syndrome/toxic epidermal necrolysis are dark red with an oozing surface. Mucous membrane involvement is present in nearly all patients and may precede skin lesions, appearing during the prodrome.
Additional findings
Other findings in Stevens-Johnson syndrome/toxic epidermal necrolysis include the following:
- Painful oral erosions cause severe crusting of the lips, increased salivation, and impaired alimentation
- Lesions have been reported in the oropharynx, tracheobronchial tree, esophagus, gastrointestinal tract, genitalia, and anus
- Involvement of the genitalia may lead to painful micturition
- Intact expectorated cylindrical casts of bronchial epithelium have been reported
- Patients may develop a profuse, protein-rich diarrhea
- Internal involvement is not necessarily limited to patients with extensive cutaneous involvement
Ocular lesions are especially problematic because they have a high risk of sequelae. Initially, the conjunctivae are erythematous and painful. The lids are often stuck together, with efforts to loosen them resulting in tearing of the epidermis. Pseudomembranous conjunctival erosions may form synechiae between the eyelids and the conjunctivae. Keratitis, corneal erosions, and a siccalike syndrome may develop.
Pharmacologic Therapy
Corticosteroid therapy
The use of corticosteroids in the management of the Stevens-Johnson syndrome/toxic epidermal necrolysis spectrum is one of the most controversial areas in Dermatology. Administration early in the course of disease has been advocated, but multiple retrospective studies demonstrate no benefit or higher rates of morbidity and mortality related to sepsis. This risk is probably proportional to the area of sloughed skin.
Halebian et al advised against the use of steroids based on 2 open, nonrandomized prospective studies of corticosteroids in 30 patients admitted to a burn unit with Stevens-Johnson syndrome or toxic epidermal necrolysis.[4] Fifteen patients received corticosteroids and 15 did not. The groups were statistically similar in terms of age, morbid days before burn center admission, and the amount of skin sloughed. Thirty-three percent of the steroid group survived, versus 66% of the nonsteroid group. Sepsis occurred with similar frequency in both groups, but 91% of patients with sepsis in the steroid group died, versus 56% of the infected patients in the nonsteroid group.
Steroids are suggested to predispose patients to gram-negative sepsis by impairing host resistance and by ultimately leading to late clinical recognition of sepsis through suppression of symptoms. Because multiple studies, albeit uncontrolled, have demonstrated a higher morbidity and mortality in patients receiving corticosteroids, most authorities do not recommend their use.
Intravenous immunoglobulin
A number of studies support the use of intravenous immunoglobulin (IVIG) in the treatment of toxic epidermal necrolysis. Viard et al suggested that apoptotic cell death occurs via activation of a cell-surface death receptor.[5] In vitro, target cell death was blocked by a receptor-ligand blocking antibody and by antibodies present in pooled human IVIG. An open trial of IVIG in 10 patients with toxic epidermal necrolysis resulted in a halt of progression within 24-48 hours, with no mortality.
Since 2000, a number of case reports and 8 noncontrolled, clinical studies containing 9 or more patients have analyzed the efficacy of IVIG in toxic epidermal necrolysis. Some studies did not demonstrate a therapeutic benefit, while others showed decreased mortality.[6, 7, 8] Six of the 8 studies suggested a benefit from IVIG administered at doses above 2g/kg.
Schneck et al published a retrospective study of patients from France and Germany enrolled in EuroSCAR, a case-control study of risk factors, and found that neither IVIG nor corticosteroids decreased mortality in comparison with supportive care alone.[9]
Given the potentially fatal nature of toxic epidermal necrolysis and the ethical issues involved, a randomized, controlled trial will likely never be performed. Given the suggestion of a therapeutic benefit, many centers are incorporating IVIG into their treatment protocols. At University Hospital at Stony Brook, New York, Stevens-Johnson syndrome/toxic epidermal necrolysis patients are treated with a dosage of 1g/kg/day for 4 consecutive days.
Cyclosporine
An open study from the trauma literature demonstrated the efficacy of cyclosporine in the treatment of toxic epidermal necrolysis. Arevalo et al presented 11 patients admitted consecutively to a burn unit, with toxic epidermal necrolysis involving a large BSA (83% ± 17%).[10] Each patient received 3mg/kg of cyclosporine daily, with the drug administered enterally every 12 hours. This group was compared to a series of 6 historical control subjects treated with cyclophosphamide and corticosteroids.
In the study, the time from the onset of skin signs to arrest of disease progression and to complete reepithelialization was significantly shorter in the cyclosporine group. All patients in the cyclosporine group survived versus 50% surviving in the cyclophosphamide group. Given a mortality rate of approximately 30% in patients not infected with human immunodeficiency virus (HIV) with toxic epidermal necrolysis, cyclosporine may prove to be a life-saving therapy, but randomized, controlled trials are needed to make definitive recommendations.
Other medications
Cyclophosphamide, N- acetylcysteine, and monoclonal antibodies directed against cytokines have been used in isolated case reports and in small, uncontrolled studies. Thalidomide has been shown to have a deleterious effect on patients' outcomes.[11]

No hay comentarios:
Publicar un comentario